Diabetic Retinopathy
What is diabetic retinopathy?
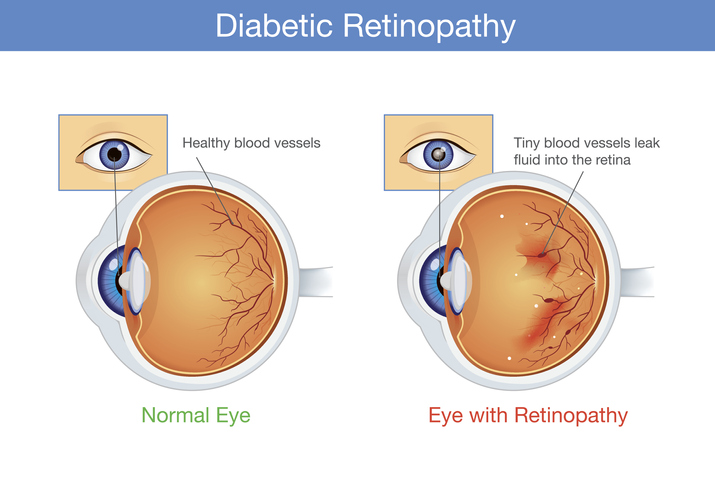
High blood sugar levels from diabetes mellitus cause damage to small blood vessels throughout the body, including in the eye. The retina is a common site of involvement. Diabetic retinopathy can be classified into two general types: nonproliferative diabetic retinopathy and proliferative diabetic retinopathy.
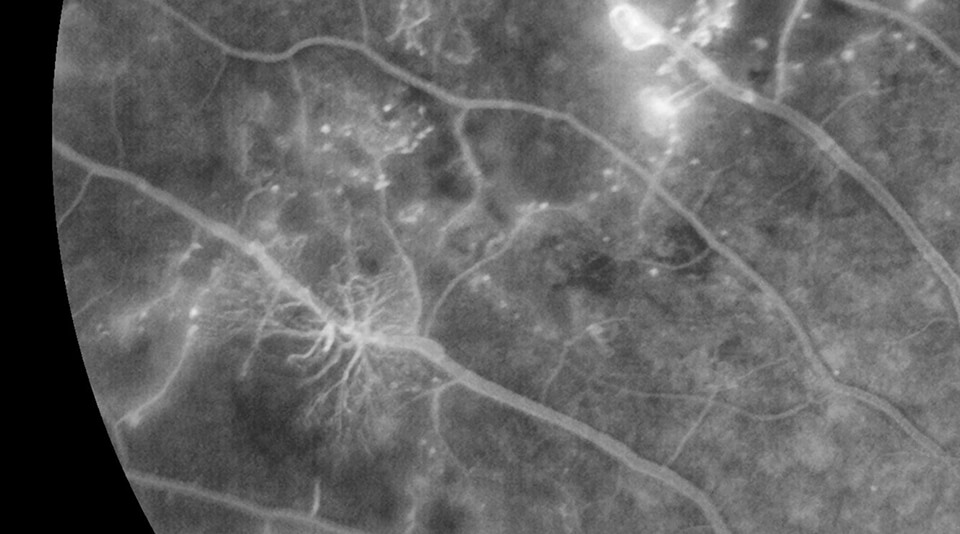
Nonproliferative Form
In the nonproliferative form, damage to small retinal blood vessels leads to microaneurysms, retinal hemorrhages, exudates, cotton wool spots, and retinal swelling (known as diabetic macular edema). Proliferative diabetic retinopathy is even more serious and is characterized by the growth of new, abnormal blood vessels that can take over the front and back of the eye. These blood vessels are fragile and can cause large hemorrhages in the eye (vitreous hemorrhage). Scar tissue can form on the surface of the retina, leading to retinal detachment. The abnormal blood vessels can also grow on the iris and clog the drainage area of the eye, leading to high eye pressures and a serious condition known as neovascular glaucoma. If left untreated, these complications can cause blindness and even loss of the eye.
What are the symptoms of diabetic retinopathy?
Proliferative Diabetic Retinopathy (PDR) can cause profound visual impairment. Patients may report hazy vision, difficulties with night vision, and floaters. It may also take a long time for eyes to adjust to changes in lighting conditions (ie, going from a dark room to the bright outdoors, or vice versa). If neovascular glaucoma develops, a patient may have a loss of vision, eye redness, and severe pain. Patients with a retinal detachment may experience loss of peripheral vision, blurred vision, flashing lights, and floaters.
Complications Caused By Diabetic Retinopathy
Diabetic retinopathy involves abnormal growth of blood vessels in the retina. This can lead to complications that can endanger your vision:
- Vitreous hemorrhage — If abnormal new blood vessels bleed into the clear, jelly-like vitreous that fills the center of your eye, this can cause a few dark spots (floaters) or it can block vision if the vitreous cavity fills completely. This doesn’t necessarily cause permanent vision damage, as the blood often clears.
- Retinal detachment — As your eye develops the abnormal blood vessels, this stimulates the growth of scar tissue. This scar tissue can tug on the retina and pull it away from the back of the eye. This can lead to severe vision loss.
- Glaucoma — If new blood vessels grow in the front of the eye, they can interfere with the normal flow of fluids out of the eye. This causes the pressure inside the eye to build, causing optic nerve damage.
- Blindness — Whether due to the diabetic retinopathy or to glaucoma that has developed because of it, the end result can be complete vision loss.
Who is at risk for developing diabetic retinopathy?
If you have diabetes, you can develop diabetic retinopathy. These factors increase your risk:
- Longer duration having diabetes
- Poor control of your blood sugar levels
- High cholesterol
- High blood pressure
- Pregnancy
- Tobacco use
- Being African American, Hispanic, or Native American
Can diabetic retinopathy be prevented?
If you have diabetes it’s not always possible to prevent developing diabetic retinopathy. There are two keys really: controlling your blood sugar and blood pressure, and having yearly eye exams with dilation. The goal is to prevent vision loss. If you’re diabetic, there are some things you can do to lower your risk of getting diabetic retinopathy:
- Manage your diabetes and blood sugar levels — Take your diabetes medicine regularly as directed. Try and eat a healthy diet and incorporate exercise into your life. You’ll need to test your blood sugar levels several times each day.
- Get an A1C test — Have your doctor call for a glycosylated hemoglobin test, or hemoglobin A1C. This details your average blood sugar level for the two to three months prior to your test. The goal is for A1C to be below 7 percent.
- Keep your blood pressure and cholesterol levels under control — Eating better and exercising regularly helps.
- Don’t smoke
- Pay attention to any vision changes — See an eye doctor if you experience any sudden vision changes or your vision becomes blurry, spotty, or hazy.
Diabetic Retinopathy Treatment Options
In the early stages of NPDR, treatment measures are focused on slowing the progression of the disease. The importance is placed on controlling blood sugar levels, blood pressure, cholesterol, and other vascular risk factors. Smoking cessation should be pursued, if applicable. Medical control of diabetes mellitus is very important in order to preserve vision and to prevent other systemic complications such as kidney disease, heart disease, stroke, and neuropathy. Working closely with a primary care provider is essential in meeting these health goals.
A variety of retinal treatment options are available if the diabetic retinopathy is more severe. Diabetic macular edema (swelling of the central retina) is managed with injections of medications into the eye and laser treatments. There are several injectable medications that are available. The most common medications are known as “anti-VEGF” agents, and they counteract the effects of a molecule inside the eye known as a vascular endothelial growth factor. The levels of VEGF are abnormally high in diabetic retinopathy and this leads to leaky retinal capillaries, macular edema, and the growth of abnormal, fragile blood vessels. In addition to anti-VEGF medications, steroid injections can be used to treat complications from diabetic retinopathy.
Proliferative diabetic retinopathy is initially managed with laser treatments and eye injections. Surgery may be necessary if more serious complications arise, such as vitreous hemorrhage, retinal detachment, and neovascular glaucoma.
Retinal Treatments
A variety of retinal treatment options are available if the diabetic retinopathy is more severe. Diabetic macular edema (swelling of the central retina) is managed with injections of medications into the eye and laser treatments. There are several injectable medications that are available.
What are some common medications I can take?
Proliferative diabetic retinopathy is initially managed with laser treatments and eye injections. Surgery may be necessary if more serious complications arise, such as vitreous hemorrhage, retinal detachment, and neovascular glaucoma.
Managing Your Proliferative Diabetic Retinopathy
Proliferative diabetic retinopathy is initially managed with laser treatments and eye injections. Surgery may be necessary if more serious complications arise, such as vitreous hemorrhage, retinal detachment, and neovascular glaucoma.
Schedule a Consultation
To learn more about diabetic retinopathy, please call (855) 515-2020 to schedule a consultation.
We are proud to serve the communities of Minneapolis/St Paul, Brainerd, Duluth, Glencoe, Mankato, St. Cloud, and more.


